Breaking News on Flora
So small and unspoken, but so important for our well-being and balance: today's topic is about the bacteria that make up our gut flora. This is the one we only think about when the doctor prescribes Floratil along with the antibiotic needed to treat our illness.
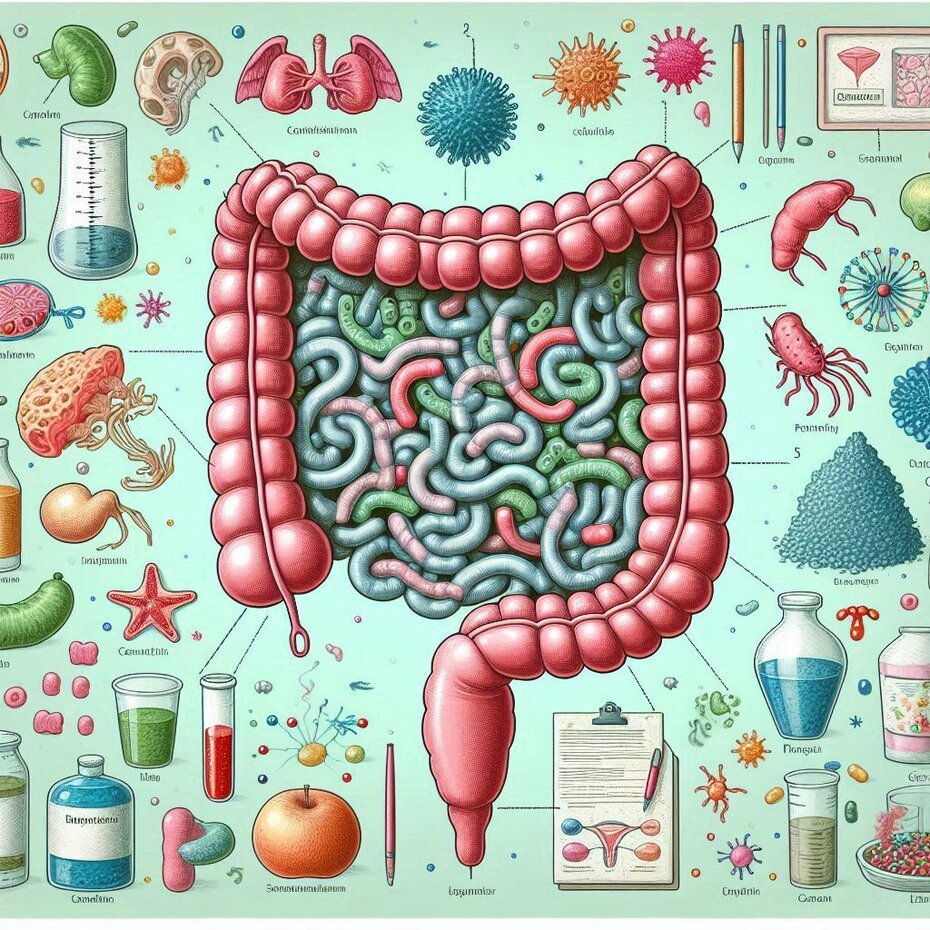
Gut flora is the popular name given to the microbiota that inhabits our intestines and is made up of bacteria, fungi, protozoa and viruses. Anyone who thinks that only the so-called 'good bacteria', those that frequent yogurt pots and probiotics, live in our beloved tummy is mistaken. Everything lives there, including the bad bacteria. But these are generally under the careful control of the rest of our gut population. But if you take an antibiotic, things can get out of control. Especially if the antibiotic is aimed at killing gram-negative bacteria.
Gram-negative bacteria have a double layer of protection on their cell walls, which makes them more difficult to kill than gram-positive bacteria. If the antibiotic you have been prescribed targets gram-negative bacteria, as is the case with amoxicillin and clindamycin, this means that gram-positive bacteria will also be wiped out, and among them the 'good bacteria' on which the balance of your microbiota depends. In other words, you will develop dysbiosis.
When the doctor prescribes a probiotic alongside the antibiotic, he aims to reduce the impact of the antibiotic treatment on your gut flora, preventing the onset of dysbiosis. And this is extremely important, as the flora participates in your digestive process, is responsible for maintaining your immune system, and its imbalance can result in metabolic and neurological diseases.
It is now known that an imbalance in the gut flora contributes to an increase in food allergies and intolerances. I'm sure you've heard someone comment in amazement about the incredible number of people who nowadays suffer from at least one of these two problems. Research on mice is helping us to understand the mechanism responsible for the appearance of these diseases.
Research with mice has been of great importance for the development of antibiotics that don't harm our gut flora, because the gut microbiota of mice is very similar to the human microbiota. The research carried out by Muñoz et alii, published in the latest Nature, reveals that the metabolites of some bacteria that make up the gut flora of mice help to maintain the integrity of their gut membrane. In cases where these bacteria are removed from the flora, the integrity of the gut membrane is reduced and it becomes permeable. With the increased permeability of the gut wall, particles that travel through the gut tract cross this membrane and enter the bloodstream, causing allergies and food intolerances.
Dysbiosis can be caused by alcohol consumption, a high-fat diet, genetic diseases or the use of antibiotics. However, regenerating the gut flora is no simple matter. It's not enough to consume probiotics, as their effect is not long-lasting.
The consumption of fermented foods and drinks such as pickles, kombucha, kefir, kimchi and others has become an increasingly common practice as a way of increasing the consumption of probiotic foods and thus maintaining the balance of the microbiota. However, if you are already suffering from dysbiosis, this can be a dangerous practice, as it is difficult to control the composition of the colony used to generate these foods, and they can be contaminated with pathogenic bacteria if the procedure adopted lacks hygiene.
The effective regeneration of flora has been achieved with a more radical and more difficult to control method: the ingestion of capsules containing fecal pellets from individuals with healthy gut flora. In other words, a pathologist examines the feces of a group of people in search of a sample rich in good bacteria, puts a sample of these feces in a capsule and asks you to swallow it. And tan dam, the treatment is complete.
Hospital-acquired Chlostridia intestinal infections are difficult to cure and occasionally lead to the patient's death, as they are resistant to most of the antibiotics currently available. However, treatments with capsules containing fecal pellets have been successful in these cases, managing to restore the patient's gut flora and fight the infection.
There is still a lot of work to be done in this area of research, but one lesson stands out: we should avoid self-medication and only take antibiotics on medical advice.
Translated with DeepL.com (free version)
Voltar